The UN World. Current guidelines from the British HIV Association BHIVA state that HIV positive mothers should be advised to formula feed exclusively from birth.

Hiv Breastfeeding And Being Undetectable Avert
The specific objectives of this study were to 1 assess HIV-positive mothers knowledge and understanding of the WHO guidelines for infant feeding in the context of HIVAIDS.
Breastfeeding options for hiv positive mothers. Mixing breastmilk and other foods before this time increases your babys risk of HIV. What to advise when mothers living with HIV do not plan to. The information available to mothers and other parents living with HIV can be confusing for those who may want to explore the option of breastfeeding feeding milk to a baby from another persons body also called nursing body feeding or chestfeeding.
Safe feeding for HIV-positive mothers Exclusive breastfeeding is defined as frequent breastfeeding on demand without giving other foods or drinks except vitamins or medicines Langley 1998. Mothers known to be HIV-infected and whose infants are HIV uninfected or of unknown HIV status should exclusively breastfeed their infants for the first 6 months of life introducing appropriate complementary foods thereafter and continue breast feeding. Exclusive breastfeeding is recommended for the first six months.
Breastfeeding is a socio-culturally acceptable universal way of feeding infant during the first year of life and a key determinant of child survival and development. 3 Breast milk only If you choose to breastfeed while your baby is less than 6 months old you should give breast milk only. When the mother chooses not to breastfeed her options of alternative feedings are the.
This means that the child can benefit from breastfeeding with very little risk of becoming infected with HIV. Feeding choices of HIV positive mothers and its impact on mother to - child transmission MTCT of HIV infection in Eastern Nigeria. The impossible dilemma faced by HIV-positive mothers is whether to breastfeed their infants in keeping with cultural norms but in doing so risk transmitting the virus through breast milk or to pursue formula feeding which comes with its own set of risks including a higher rate of infant mortality from diarrheal illnesses while reducing transmission of HIV.
Because of the very low risk of mother-to-child HIV infection BHIVA guidelines advise that mothers who choose to breastfeed should be supported to do so. HIV positive mothers are encouraged to breastfeed but should not default on their antiretroviral medication and vitamin supplements. Treatment of mothers andor their infants with.
HIV-positive women still confused about infant-feeding choices. Among women and other birthing parents living with HIV infant-feeding choices are even more complex and feature unique challenges. Even if you are taking your HIV medication your baby has double the chance of becoming infected with HIV if you breastfeed for 12 months rather than stopping before your baby is 6 months old.
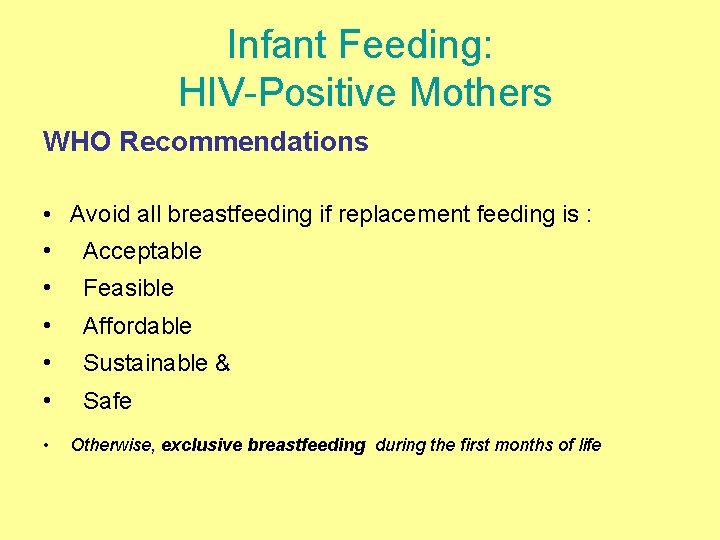
Deciding which path to follow requires a lot of thought as this is a long-term decision that spans a. A Acceptable F Feasible A Affordable S Safe S Sustainable. In settings where national health authorities are recommending breastfeeding for HIV-infected mothers.
These mothers may need ongoing feeding guidance andor emotional support. For HIV positive mothers in developing countries complete avoidance of breastfeeding may not be a safe option due to cost lack of safe water unsanitary conditions and socio-cultural factors. HIV-positive mothers and family members fathers and grandmothers of the infant feeding options for HIV infected mothers in Ghana.
This option is chosen on the following AFASS criteria. Breastfeeding 1 while a multi-layered and morally charged issue is considered the healthiest option for infant feeding for the general population. The latest guidelines on infant-feeding options for HIV-positive mothers in Africa have not been disseminated in many countries leaving women dangerously confused about the best nutritional path to protect their children from contracting the virus a new report shows.
If the mother is HIV positive the newborn will By Hlulani Masingi As we enter the festive season and acknowledge World AIDS Day on 1st December many mothers might be wondering how safe breast milk is. In India if HIV positive Mothers from high income families choose not to breastfeed replacement feeding can be advocated. Exclusive or only breastfeeding means that the mother gives her baby breastmilk only.
Breastfeeding options for mothers who have HIV positive from this safe breastfeeding wet nursing and heat-treated breast milk are best one. In resource-limited settings such as some parts of Africa the World Health Organization WHO recommends that HIV-infected mothers breastfeed exclusively for the first 6 months of life and continue breastfeeding for at least 12 months with the addition of complementary foods. Exclusive breastfeeding and exclusive formula feeding both of which have cons and pros but on no condition should the feeding options be combined.
Since 2010 the World Health Organization recommends lifelong antiretroviral treatment for all women living with HIV and exclusive breastfeeding for six-months followed by breastfeeding until 24-months for all HIV positive mothers. The conditions are that mothers follow the antiretroviral therapy ART strictly and that standard HIV. Mixed feeding can be defined as breastfeeding and giving any other liquids for example water juice tea solids or milks formula or animal.
About one hundred and four 104 pregnant HIV positive mothers attending the PMTCT ante-natal clinic were counseled during their pregnancy through their labor and breastfeeding period and recruited for the. Interventions to support infant feeding practices by mothers living with HIV2 22. What Are Safe Feeding Options In The Face Of HIV.
For the first time WHO is recommending that HIV-positive mothers or their infants take antiretroviral drugs throughout the period of breastfeeding and until the infant is 12 months old. This means that her baby gets no water colicwind medication tea juice other milk or solid foods. If you do breastfeed you must always take your treatment and exclusively breastfeed give breastmilk only for at least six months.
Feeding an HIV-exposed infant can be very tricky. The duration of breastfeeding by mothers living with HIV1 12. Prescribed medication must however be given.
What to advise when mothers living with HIV do not exclusively breastfeed3 28. Semi-structured interviewer-administered questionnaire was used in the cross-sectional survey to obtain data from 600 HIV positive mothers to assess practices regarding infant feeding choices and factors influencing these choice. Current World Health Organization guidance on HIV and infant feeding is clear that for most mothers in most countries exclusive breastfeeding for the first six months followed by continued partial breastfeeding for at least the first year of life will enhance HIV-free child survival.
There are two feeding options available.
What Works Safe Motherhood And Prevention Of Vertical Transmission Postpartum

Ten Safer Breastfeeding Rules For Women Living With Hiv Aidsmap

Women Living With Hiv In High Income Settings And Breastfeeding Moseholm 2020 Journal Of Internal Medicine Wiley Online Library

Enrolment Of Hiv Positive Mothers And Follow Up Of Their Infants A Rt Download Scientific Diagram
Infant Feeding And Hiv Dr Kanupriya Chaturvedi Dr